When your kidneys start to fail, they don’t just stop filtering waste-they also lose their ability to keep your sodium levels in check. That’s when problems like hyponatremia and hypernatremia creep in. These aren’t just lab numbers gone wrong. They’re serious, life-threatening conditions that affect nearly 1 in 4 people with advanced kidney disease. And most patients, even those under regular care, don’t realize how dangerous these imbalances can be until it’s too late.
What Exactly Are Hyponatremia and Hypernatremia?
Hyponatremia means your blood sodium level is below 135 mmol/L. Hypernatremia is the opposite-above 145 mmol/L. Sodium isn’t just table salt. It’s the main electrolyte that controls how much water is in and around your cells. When sodium drops too low, water floods into your brain cells. When it spikes too high, your cells shrink. Both can cause confusion, seizures, coma, or death.
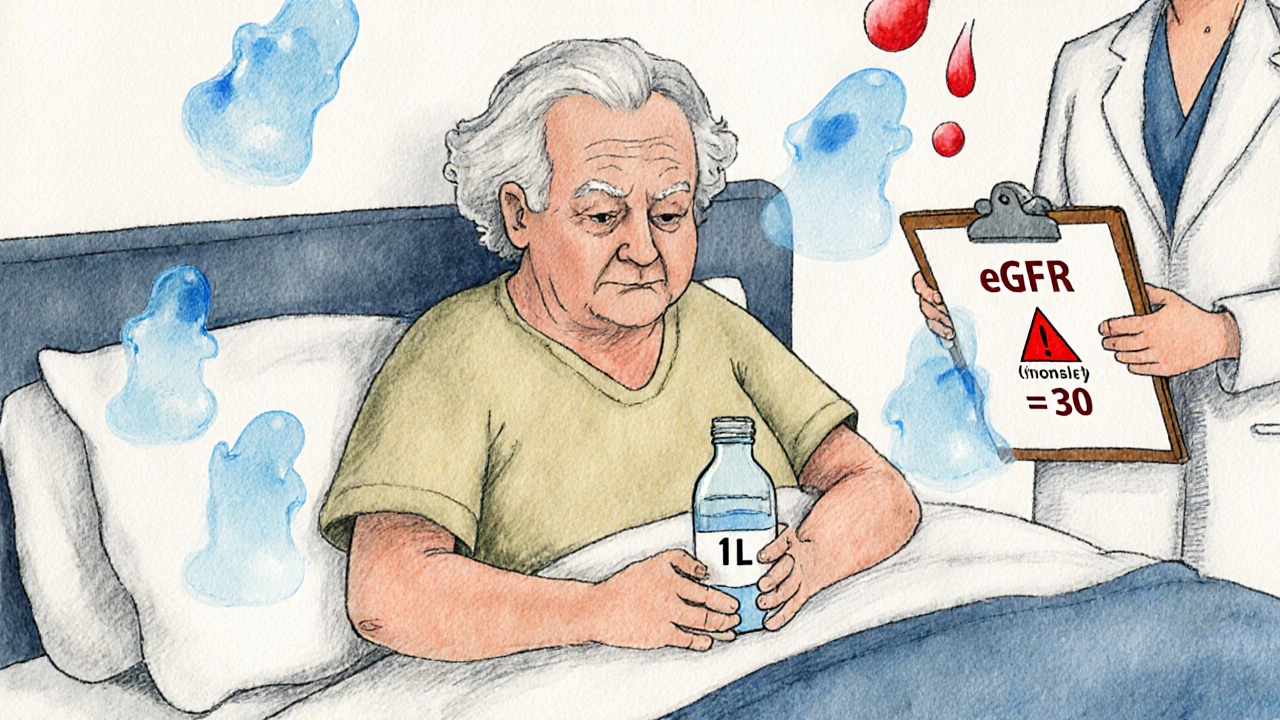
In healthy people, your kidneys adjust urine output to keep sodium stable. But in chronic kidney disease (CKD), that system breaks down. By stage 4 or 5, when your kidney function drops below 30 mL/min/1.73m², your kidneys can’t make enough dilute urine to flush out extra water-or enough concentrated urine to hold onto water when you’re dehydrated. That’s why sodium levels swing wildly in CKD patients, even if they eat and drink normally.
Why Kidney Disease Makes Sodium Imbalance Worse
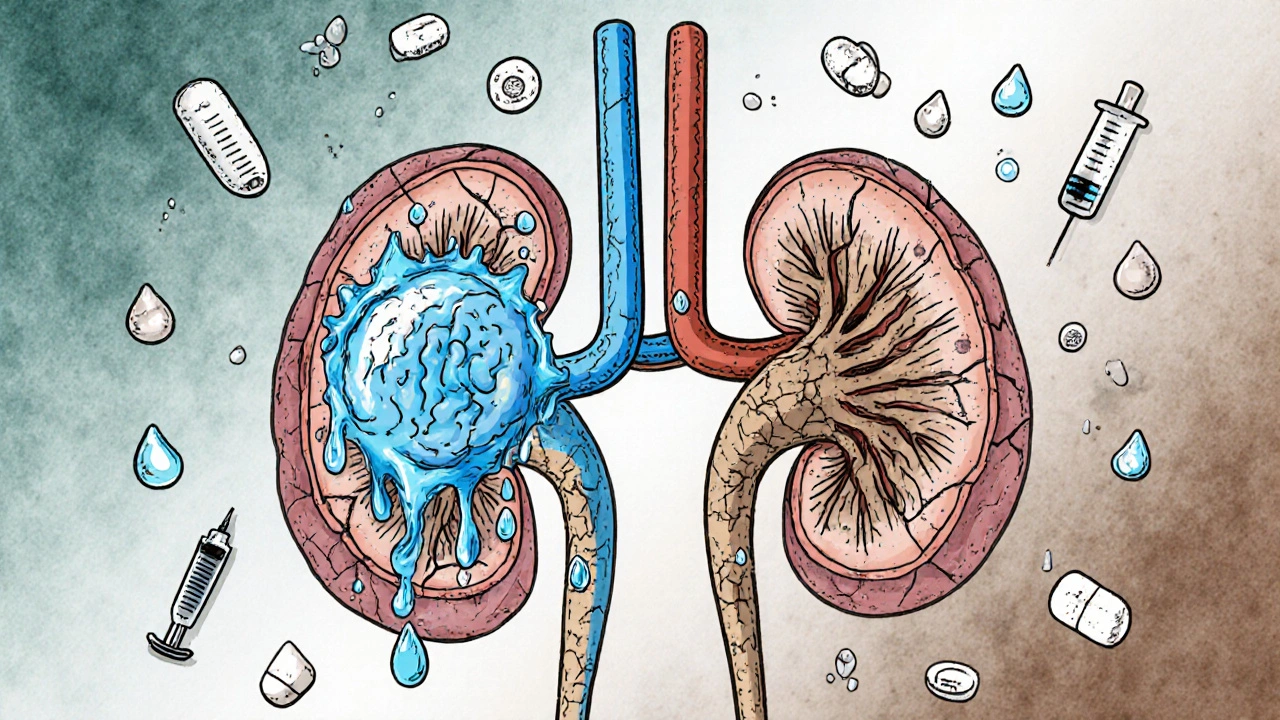
Your kidneys handle sodium in two ways: by filtering it out and by reabsorbing it back into the blood. As kidney damage progresses, fewer nephrons are left to do the job. To compensate, each remaining nephron tries to reabsorb more sodium. But this system is slow, inefficient, and easily overwhelmed.
Here’s what happens in real life:
- Early CKD (stages 1-2): You can still excrete sodium, but you need to pee more to do it. Drink too much water? Your kidneys can still handle it.
- Mid-stage CKD (stages 3-4): Your kidneys start struggling. A 1.5-liter water intake that was fine last year now causes swelling and low sodium.
- Advanced CKD (stage 5): Even 800 mL of water a day can push you into hyponatremia. And if you’re not drinking enough? You risk hypernatremia fast.
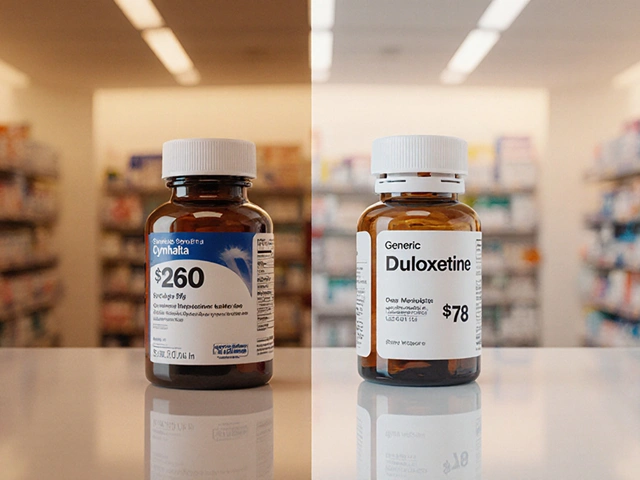
Plus, many CKD patients are on diuretics. Thiazides-commonly prescribed for high blood pressure-are especially risky. They block sodium reabsorption in the kidneys, but in advanced CKD, they don’t work well and instead cause dangerous sodium loss. That’s why the FDA warns against using thiazides when eGFR is below 30.
Types of Hyponatremia in Kidney Disease
Not all low sodium is the same. It’s classified by body fluid volume:
- Euvolemic hyponatremia (60-65% of cases): Your total body water is high, but your blood volume looks normal. This is the most common type in CKD. It’s caused by your kidneys being unable to excrete water, often worsened by thiazides or SIADH (a condition where your body makes too much ADH hormone).
- Hypervolemic hyponatremia (15-20%): You have fluid overload-swollen legs, shortness of breath, weight gain. This happens with end-stage kidney disease or heart failure. The extra fluid dilutes your sodium.
- Hypovolemic hyponatremia (15-20%): You’ve lost sodium and water, but lost more sodium. This can come from vomiting, diarrhea, or salt-wasting syndromes like milk-alkali syndrome or overuse of diuretics.
Here’s the catch: In CKD, it’s hard to tell which type you have just by looking at swelling or weight. Blood tests and urine sodium levels are needed. Many doctors miss this and treat all hyponatremia the same-leading to dangerous mistakes.
Hypernatremia in Kidney Disease: The Hidden Danger
Most people focus on low sodium. But high sodium is just as deadly-and often overlooked. Hypernatremia in CKD usually happens when patients can’t drink enough water. Elderly patients, those with dementia, or people on strict fluid limits are at highest risk.
When kidneys can’t concentrate urine, they lose more water than sodium. So even if you’re drinking a little, your body is still dehydrating. A 70-year-old with stage 4 CKD who’s told to drink only 1 liter a day might not feel thirsty. But over 2-3 days, their sodium climbs. They get confused. They stop eating. They collapse.
Correction is tricky. Dr. Richard H. Sterns, a leading nephrologist, says: “The most common error is rushing to fix hypernatremia too fast.” Lowering sodium by more than 10 mmol/L in 24 hours can cause brain swelling. The fix? Slow, controlled water replacement-oral if possible, IV if needed-with constant monitoring.
How Dangerous Are These Conditions?
Hyponatremia isn’t just a lab abnormality. It’s a death marker.
- People with mild hyponatremia in CKD have a 1.94 times higher risk of dying.
- Those hospitalized with low sodium have 28% higher mortality than those with normal levels.
- Hyponatremia increases fall risk by 82% and fracture risk by 67%-especially in older adults with weak bones.
- Cognitive decline is 1.35 to 2.17 times more likely in people with chronic low sodium.
Hypernatremia is even worse. Studies show mortality rates jump to over 40% in hospitalized patients with sodium above 155 mmol/L. And it’s often missed until the patient is unresponsive.
Here’s a hard truth: In advanced CKD, sodium levels are one of the best predictors of survival-better than creatinine or eGFR alone.
Treatment: What Actually Works
There’s no one-size-fits-all fix. Treatment depends on type, speed of onset, and kidney function.
For Hyponatremia
- Fluid restriction: The first step. For early CKD, 1,000-1,500 mL/day. For advanced CKD, drop to 800-1,000 mL/day. Many patients don’t realize how little that is-about 3-4 cups.
- Stop thiazides: If you’re on hydrochlorothiazide or chlorthalidone and have eGFR below 30, ask your doctor to switch you to a loop diuretic like furosemide.
- Sodium supplements: Only for salt-wasting syndromes. Doses of 4-8 grams of sodium chloride per day can help, but only under close supervision.
- Never use vaptans: Drugs like tolvaptan that block ADH are banned in advanced CKD. Your kidneys can’t respond to them, and they can cause liver damage or rapid sodium shifts.
For Hypernatremia
- Slow water replacement: Correct sodium by no more than 10 mmol/L in 24 hours. Use oral water if possible. IV fluids only if the patient can’t drink.
- Check medications: Anticholinergics, lithium, and some psychiatric drugs can reduce thirst. Review all meds with your doctor.
- Address the root cause: Is the patient unable to access water? Do they have dementia? Are they on too-restrictive fluid limits? Fix the environment, not just the number.

What Patients Get Wrong
Most patients with CKD are told to eat low-sodium, low-potassium, low-protein diets. That’s good-for potassium and acidosis. But here’s the trap:
When you cut out protein and salt, you reduce the solute load your kidneys need to flush. That sounds smart. But your kidneys need solutes to pull water out. Less solute = less urine = water builds up = hyponatremia.
A 2023 Japanese study found that patients on strict solute-restricted diets had 30% higher rates of hyponatremia. One patient, a 68-year-old woman with stage 4 CKD, ate only 1,000 calories a day, mostly vegetables and water. Her sodium dropped to 128 mmol/L. She fell, broke her hip, and died. Her diet was “healthy”-but deadly for her kidneys.
Another mistake: thinking “no salt” means no sodium at all. Many patients avoid table salt but still eat bread, canned soup, or processed foods with hidden sodium. Others, terrified of high sodium, drink nothing but water and end up with hypernatremia.
What Works in Real Life
Successful management isn’t about rules-it’s about personalization.
- Work with a renal dietitian. Most patients need 3-6 sessions to understand fluid and sodium balance.
- Use a daily log: Record fluid intake, weight, and symptoms like swelling or confusion.
- Check sodium every 2-4 weeks if you’re in stage 4 or 5 CKD. Don’t wait for symptoms.
- Ask about the new sodium monitoring patch approved by the FDA in 2023. It measures sodium in your skin fluid continuously and alerts you to trends before your blood level drops.
- Build a care team: Nephrologist, dietitian, pharmacist, and primary care doctor must communicate. Studies show integrated care cuts hospitalizations by 35%.
The Future: What’s Changing
The 2024 KDIGO guidelines are expected to shift from fixed fluid limits to personalized targets based on your residual kidney function. One emerging idea: instead of telling everyone to drink 1 liter, measure how much urine you make. If you’re still making 500 mL/day, you can probably drink more. If you’re making less than 200 mL, you’re in danger.
Researchers are also studying the gut-kidney axis. New data suggests your intestines may help compensate for failing kidneys by absorbing or excreting sodium. If this is proven, future treatments might target gut bacteria or enzymes-not just fluids and pills.
For now, the message is clear: Sodium balance in kidney disease isn’t about diet alone. It’s about how your kidneys respond, what medications you take, how much you drink, and whether your care team understands the unique risks of CKD. Ignoring it can kill you. Managing it right can give you years.
Can drinking too much water cause hyponatremia in kidney disease?
Yes. In advanced kidney disease, your kidneys can’t get rid of excess water fast enough. Drinking even 1.5 to 2 liters a day-what’s considered normal for healthy people-can flood your system and lower sodium to dangerous levels. Patients with stage 4 or 5 CKD are often advised to limit fluids to 800-1,000 mL per day to avoid this.
Is low sodium more dangerous than high sodium in kidney disease?
Both are dangerous, but hyponatremia is more common and often missed. It’s linked to higher long-term mortality, falls, fractures, and cognitive decline. Hypernatremia is rarer but has a higher immediate death rate-especially if not treated slowly. Neither should be ignored.
Should I avoid salt completely if I have kidney disease?
No. Avoiding all sodium can backfire. Your kidneys need some solutes to excrete water properly. Too little salt and protein reduces your urine output, making hyponatremia more likely. The goal is balance-not elimination. Work with a renal dietitian to find your safe range, usually 1,500-2,300 mg per day, adjusted for your kidney function.
Can diuretics cause hyponatremia in kidney disease?
Yes, especially thiazides like hydrochlorothiazide. They’re less effective in advanced CKD and cause more sodium loss than water loss, leading to hyponatremia. If your eGFR is below 30, your doctor should switch you to a loop diuretic like furosemide, which works better and is safer at that stage.
How often should I check my sodium levels if I have CKD?
If you’re in stage 3 CKD, check every 3-6 months. In stage 4 or 5, check every 2-4 weeks, especially if you’re on diuretics, have swelling, or feel confused or weak. Many hospitals now use home monitoring tools or wearable patches that track sodium trends between visits.
Can hyponatremia be reversed in kidney disease?
Yes, but slowly. Rapid correction can cause osmotic demyelination syndrome, a severe brain injury. Correction should be no faster than 4-6 mmol/L in 24 hours. Most patients improve with fluid restriction, stopping harmful medications, and dietary adjustments. In some cases, especially if caught early, sodium levels return to normal without permanent damage.
What’s the biggest mistake doctors make with sodium in CKD?
Applying standard hyponatremia protocols designed for healthy people. CKD patients have reduced kidney function, so they can’t excrete water or correct sodium the same way. Giving too much IV fluid or correcting sodium too fast leads to brain damage. The key is recognizing that CKD changes everything-even basic electrolyte rules.





5 Comments
Ram tech November 15, 2025
bro i had stage 4 ckd and drank 2l of water a day like a healthy person. turned into a walking zombie for a week. doc said my sodium was 129. i thought i was being smart. turns out i was just dumb. now i drink like a camel in the desert. 800ml max. dont be me.
Jenny Lee November 15, 2025
fluid restriction is the real villain here. no one tells you how hard it is to watch everyone else drink soda while you sip 100ml of water over 4 hours. it’s not just medical-it’s emotional.
Kevin Jones November 16, 2025
the pathophysiological disconnect between solute-driven diuresis and nephron depletion in CKD creates a homeostatic vacuum where osmotic equilibrium collapses-especially under thiazide-induced sodium wasting. vaptans are contraindicated not because they’re toxic, but because the renal tubules have lost their receptor plasticity. we’re managing a failing engine with a bicycle pump.
Premanka Goswami November 16, 2025
they don’t want you to know this but the FDA banned vaptans because Big Pharma doesn’t profit from water. they make billions off dialysis and meds. your sodium imbalance? it’s a business model. the ‘patch’ they’re pushing? it’s a tracking tool for insurance surveillance. drink less. trust no one. the system is rigged.
Erica Lundy November 18, 2025
There is a profound existential paradox embedded in the management of sodium in chronic kidney disease: the body, in its desperate attempt to preserve homeostasis, becomes the architect of its own unraveling. The kidneys, once silent sentinels of balance, now labor under the weight of compromised nephrons, each reabsorption a quiet surrender to entropy. We prescribe fluid limits as if they were moral boundaries, yet the patient’s thirst remains a biological imperative, unyielding and unjudged. To restrict water is to deny the body’s most primal language. To permit it is to invite catastrophe. The tragedy lies not in the numbers-135, 145-but in the silence between them, where human beings are reduced to lab values, and the only cure is a kind of exquisite, daily surrender to uncertainty. Perhaps the real treatment is not in the algorithm, but in the compassion that acknowledges the weight of that silence.