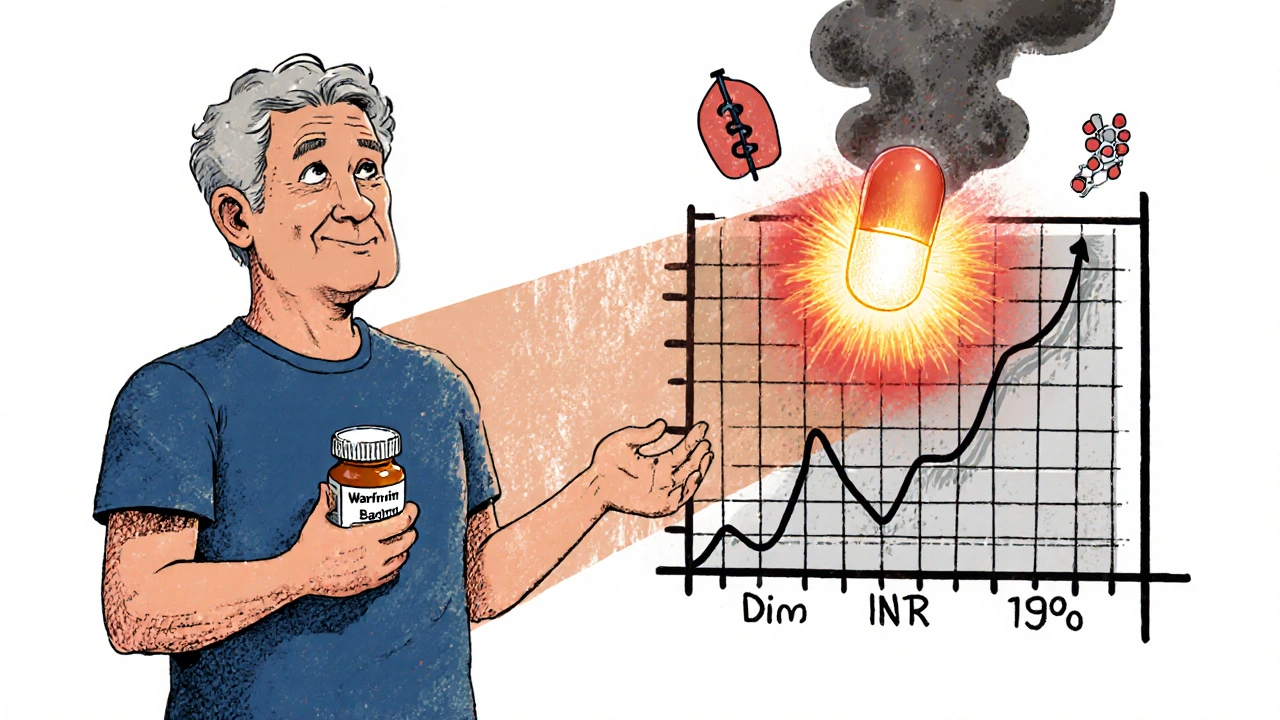
When you're on warfarin, even a simple course of antibiotics can throw your blood thinning off balance. It’s not a myth-it’s a real, well-documented risk that happens more often than you think. About one in five people taking warfarin will need an antibiotic in a given year. And for many, that leads to a sudden spike in INR, the number doctors use to measure how long your blood takes to clot. Too high, and you risk dangerous bleeding. Too low, and you could get a clot. The key isn’t avoiding antibiotics-it’s knowing which ones to watch for and how to respond.
Why Antibiotics Affect Warfarin
Warfarin doesn’t work in isolation. It’s a delicate balancing act, and antibiotics can mess with it in three main ways. First, some antibiotics block the liver enzyme CYP2C9, which breaks down warfarin. When that enzyme slows down, warfarin builds up in your blood. Second, antibiotics kill off good bacteria in your gut that make vitamin K. Since warfarin works by blocking vitamin K, less vitamin K means stronger blood thinning. Third, some antibiotics compete with warfarin for protein binding in your blood, temporarily making more warfarin available to act.This isn’t theoretical. A 2012 study of over 128,000 older adults found that anyone taking an antibiotic while on warfarin had more than double the risk of bleeding serious enough to land them in the hospital. And it’s not all antibiotics-the risk varies wildly depending on the drug.
High-Risk Antibiotics: The Ones That Can Really Spike Your INR
Some antibiotics are known troublemakers. The biggest red flag is trimethoprim-sulfamethoxazole (Bactrim, Septra). It hits all three mechanisms at once: it strongly blocks CYP2C9, wipes out gut bacteria, and displaces warfarin from proteins. Studies show it can raise INR by 1.5 to 3 units-sometimes in just 48 hours. Many patients need to cut their warfarin dose by 25% to 50% when starting Bactrim. In some cases, skipping one dose of warfarin is advised.Fluconazole, an antifungal often prescribed for yeast infections, is another high-risk player. It’s not technically an antibiotic, but it behaves like one in this context. It also inhibits CYP2C9 and has been linked to a 2.15 times higher risk of major bleeding in warfarin users.
Other high-risk drugs include metronidazole and fluoroquinolones like ciprofloxacin and levofloxacin. These are common for urinary tract infections, sinus infections, and even some pneumonia cases. If you’re on warfarin and your doctor prescribes one of these, expect your INR to climb within a few days.
Moderate-Risk Antibiotics: Proceed with Caution
Many common antibiotics fall into the moderate-risk category. These include penicillins like amoxicillin, macrolides like azithromycin (though less so than erythromycin), and cephalosporins like ceftriaxone. They don’t block CYP2C9 as strongly, but they still reduce vitamin K production in the gut. That’s enough to bump your INR by 0.5 to 1.5 units in many people.Here’s the catch: you might not feel anything. No bruising, no nosebleeds, no dark stools. But your INR could still be climbing. That’s why monitoring matters more than symptoms. A 2014 study of nearly 40,000 patients found that even though INR levels rose with these antibiotics, most patients didn’t need a dose change-unless they were checked.
Low-Risk Antibiotics: Safer Options
Good news: not all antibiotics are dangerous with warfarin. Clindamycin has almost no interaction. It doesn’t affect CYP2C9, doesn’t kill off vitamin K-producing bacteria much, and doesn’t displace warfarin. For this reason, dentists often prefer clindamycin over amoxicillin for patients on warfarin needing antibiotic prophylaxis.Azithromycin (Zithromax) is another low-risk option. Unlike erythromycin, it doesn’t significantly inhibit liver enzymes. It’s commonly used for respiratory infections and is often a safe alternative if you need a macrolide.
Even doxycycline, a tetracycline antibiotic, has minimal interaction risk. It’s often used for Lyme disease or acne and can be a reasonable choice if you’re on warfarin and need long-term treatment.
The Odd One Out: Rifampin
Most antibiotics make warfarin stronger. But rifampin does the opposite. It’s a powerful inducer of CYP2C9, meaning it speeds up how fast your body breaks down warfarin. This causes your INR to drop-sometimes dramatically. If you’re on rifampin for tuberculosis or a stubborn infection, your warfarin dose may need to go up by 50% or more to stay in range.The problem? It takes weeks for rifampin to fully kick in. So your INR might look fine at first, then suddenly crash after 7 to 10 days. This is why you need INR checks every 1 to 2 weeks while on rifampin. Stopping rifampin can be just as dangerous: your INR will rise as the enzyme induction fades, and you’ll need to lower your warfarin dose again. It’s a slow dance that requires constant monitoring.
What to Do When You Need an Antibiotic
Don’t panic. Don’t skip the antibiotic. But do this:- Check your INR before starting-get a baseline reading.
- Get it checked again within 3 to 5 days after starting the antibiotic. For high-risk drugs like Bactrim, check at day 3. For moderate ones, day 5 is fine.
- Don’t adjust your warfarin dose yourself. Talk to your anticoagulation clinic or doctor. They’ll decide if you need a reduction, increase, or no change.
- Watch for signs of bleeding: unusual bruising, pink or red urine, black or tarry stools, headaches, dizziness, or prolonged bleeding from cuts.
- Inform every provider-dentist, ER doctor, pharmacist-that you’re on warfarin. Many don’t know the risks.
A 2023 review from the University of California San Diego says: “Most patients can safely take antibiotics while on warfarin, as long as their INR is monitored.” That’s the bottom line. You don’t need to avoid antibiotics. You need to plan for them.
Special Cases: Dental Work and Surgery
If you’re scheduled for a dental procedure, your dentist might prescribe an antibiotic to prevent infection. For patients on warfarin, clindamycin is often the first choice. Avoid amoxicillin unless your INR is stable and you’re being monitored closely.For surgery, the rules are the same. Don’t stop warfarin unless your surgeon and anticoagulation team agree. Stopping warfarin increases your risk of stroke or clotting, especially if you have a mechanical heart valve. Instead, monitor INR before and after the procedure. Most patients can continue warfarin with no changes if their INR is in range.
What Research Really Says
There’s a lot of noise out there. One study says antibiotics are dangerous. Another says the risk is low. The truth? Both are right. The absolute risk of bleeding is still small for most people. But the relative risk jumps significantly with certain drugs. That’s why guidelines don’t say “avoid all antibiotics.” They say: “Know which ones are risky, check INR early, and adjust if needed.”The American Heart Association’s 2022 guidelines put it plainly: “Antibiotics can alter the anticoagulant effect of warfarin, but discontinuation of either drug is rarely necessary.” It’s about smart management, not fear.
Bottom Line: Monitor, Don’t Panic
Warfarin and antibiotics can coexist safely-if you’re prepared. The biggest mistake is assuming nothing will change. The second biggest mistake is stopping your warfarin because you’re scared.Take action: if you’re on warfarin and your doctor says you need an antibiotic, ask: “Is this one on the high-risk list?” Then schedule your INR check before you even pick up the prescription. Most clinics will do it same-day if you call ahead.
And remember: if you’re feeling fine, that doesn’t mean your INR is fine. Bleeding can happen without warning. That’s why the numbers matter more than how you feel.
Can I take amoxicillin while on warfarin?
Yes, you can take amoxicillin while on warfarin, but it’s not risk-free. Amoxicillin is considered a moderate-risk antibiotic because it can reduce vitamin K production in your gut and slightly slow down how your body breaks down warfarin. This may cause your INR to rise by 0.5 to 1.5 units. Check your INR 5 to 7 days after starting amoxicillin. Your doctor may recommend lowering your warfarin dose by 10% to 25% if your INR climbs too high.
Is Bactrim safe with warfarin?
No, Bactrim (trimethoprim-sulfamethoxazole) is one of the most dangerous antibiotics to take with warfarin. It can cause your INR to spike by 1.5 to 3 units in just a few days, greatly increasing your risk of serious bleeding. Many patients need to reduce their warfarin dose by 25% to 50% or even skip one dose. Always check your INR within 3 days of starting Bactrim. Never start Bactrim without talking to your anticoagulation clinic first.
How long after starting an antibiotic should I check my INR?
For high-risk antibiotics like Bactrim or fluconazole, check your INR within 3 days. For moderate-risk ones like amoxicillin, ciprofloxacin, or azithromycin, check at 5 to 7 days. For low-risk antibiotics like clindamycin, you can stick to your regular schedule unless you notice signs of bleeding. Always check before starting a new antibiotic to get a baseline.
Should I stop taking warfarin if I need an antibiotic?
No, you should almost never stop warfarin just because you’re taking an antibiotic. Stopping warfarin increases your risk of stroke, heart attack, or a blood clot in your lungs or legs-especially if you have a mechanical heart valve or atrial fibrillation. The better approach is to monitor your INR closely and adjust your warfarin dose under medical supervision. Your doctor may lower your dose temporarily, but stopping entirely is rarely the right move.
What antibiotics are safest with warfarin?
Clindamycin and azithromycin are among the safest antibiotics to take with warfarin. Clindamycin has almost no interaction with warfarin and is often preferred for dental procedures. Azithromycin doesn’t significantly affect liver enzymes or vitamin K levels. Doxycycline is also low-risk. Always confirm with your provider, but these are generally the go-to choices when you need an antibiotic while on warfarin.
Can rifampin be taken with warfarin?
Yes, but it’s complicated. Rifampin makes your body break down warfarin much faster, which lowers your INR and increases your risk of clots. You’ll likely need to increase your warfarin dose by 50% or more. INR levels can drop slowly over 7 to 10 days, so check your INR every 1 to 2 weeks while on rifampin. When you stop rifampin, your INR will rise again, and you’ll need to reduce your warfarin dose. This process can take 6 to 8 weeks to fully stabilize.
Next Steps: Stay in Control
If you’re on warfarin, keep a list of all your medications-including over-the-counter drugs and supplements-and share it with every provider. Ask your pharmacist to flag any new antibiotic for potential warfarin interactions. Set a reminder on your phone to check your INR 3 to 5 days after starting any new antibiotic. And never ignore a follow-up appointment-those checks are what keep you safe.Warfarin isn’t outdated. It’s still essential for millions. Antibiotics aren’t the enemy. But together, they demand attention. With the right monitoring, you can take both safely-and avoid the hospital.


11 Comments
Erika Hunt November 23, 2025
Okay, I just read this whole thing, and I have to say-I’m shocked how many people don’t know this stuff. I’ve been on warfarin for six years now, and my anticoagulation clinic literally gives me a printed cheat sheet every time I get a new script. But my cousin? She took Bactrim for a UTI last year, didn’t check her INR, and ended up in the ER with a subdural hematoma. It’s not dramatic-it’s just... basic. Like, if you’re on blood thinners, you don’t just take antibiotics like they’re Advil. And why do doctors still prescribe Bactrim without warning? It’s not even the first-line choice anymore. I mean, come on. We’ve had data since 2012. Why is this still a surprise?
Also, I love that they mentioned clindamycin for dental work. My dentist always asks me if I’m on warfarin, and then says, “We’ll use clindamycin,” and I just breathe a sigh of relief. Like, thank you, Dr. Patel, for knowing your stuff. I wish more providers did. I’ve had two ER visits because some nurse didn’t know rifampin could drop INR-so now I carry a laminated card in my wallet. It says: “I’m on warfarin. Do not give me Bactrim, fluconazole, or metronidazole without checking INR.” I even have a QR code that links to the 2023 UCSD review. It’s extra, but it’s saved me twice.
And yes, azithromycin is the MVP. I had pneumonia last winter and begged for it instead of cipro. My doctor was like, “Really?” and I was like, “Yes, really. I’m not dying for a faster cure.” It worked. No INR spike. No drama. Just me, my tea, and my phone reminder to check my INR on day five. Which, by the way, I set to go off at 8 a.m. every day. I don’t trust my memory anymore. I used to be the person who said, “I’ll remember,” and then I forgot. Now? I have alarms. For everything. I even have one for when my warfarin bottle is half empty. I’m not crazy. I’m just... prepared.
Also, I’m so tired of people saying “just stop warfarin.” No. No, no, no. If you have AFib or a mechanical valve, stopping warfarin is like removing the seatbelt from a car going 70 mph. You might not crash tomorrow. But the risk isn’t theoretical. It’s in the data. And if you’re thinking, “I’ll just take aspirin instead,” please, for the love of all that is holy, don’t. Aspirin doesn’t protect you the same way. I’ve seen the studies. I’ve read the guidelines. I’ve cried in the clinic waiting room because I was scared. But I didn’t stop. I adjusted. I monitored. I lived. And you can too.
So if you’re reading this and you’re on warfarin? Don’t panic. Just... be a little more paranoid than you think you need to be. And if you’re a provider? Please, for the love of medicine, just ask. Ask about warfarin. Ask about INR. Don’t assume. Don’t guess. Just ask. It’s not hard. It’s just... necessary.
Sharley Agarwal November 23, 2025
Stop giving people antibiotics like candy.
prasad gaude November 25, 2025
It’s funny, isn’t it? We live in a world where we can map the human genome, yet we still treat warfarin like some ancient curse whispered in the dark. Antibiotics? They’re just molecules. Warfarin? Just another molecule. But we give them gods and demons. We fear Bactrim like it’s a dragon, and praise clindamycin like it’s a saint. But the truth? The body doesn’t care about brand names. It cares about enzymes. About vitamin K. About half-lives. About kinetics. We’ve turned a biochemical balance into a moral dilemma. We’re not just managing drugs-we’re managing fear. And that’s the real infection.
My grandfather took warfarin for 17 years. He never checked his INR after antibiotics. He didn’t have a clinic. He didn’t have a phone reminder. He had his wife, and her memory. And he lived. Not because he was lucky. But because he was humble. He didn’t fight the science. He listened. He adapted. We’ve lost that. We want apps, alerts, QR codes, laminated cards. But the real wisdom? It’s in the quiet. In the asking. In the not-knowing. And then, listening.
So yes, check your INR. But also, check your arrogance. The body doesn’t need more control. It needs more respect.
Timothy Sadleir November 27, 2025
Let me be perfectly clear: this entire article is a product of pharmaceutical lobbying disguised as medical advice. The real reason you're being told to monitor INR with antibiotics is because the anticoagulation industry needs you to come in for weekly blood draws. That’s how they make money. Did you know that the INR testing market is worth over $12 billion annually? And who benefits? Not you. The clinics. The labs. The corporations that sell the test strips. The FDA? They don’t care. They’re too busy approving new anticoagulants that cost $10,000 a year. Meanwhile, you’re being told to avoid Bactrim because it’s ‘dangerous’-but what about the fact that amoxicillin is just as likely to cause bleeding in elderly patients with renal impairment? Why isn’t that in the article? Why is the narrative so one-sided? This isn’t medicine. It’s marketing. And you’re the product.
And don’t even get me started on rifampin. That’s a tuberculosis drug. Why are you even prescribing it to someone on warfarin unless you’re trying to kill them? It’s not an interaction-it’s a death sentence disguised as a treatment protocol. And yet, here we are, being told to ‘adjust’ and ‘monitor.’ That’s not safety. That’s negligence dressed in white coats.
And the worst part? You’re being told to ‘ask your doctor.’ But your doctor doesn’t know. They’re reading this same article. And they’re just as confused as you are. The system is broken. And no amount of laminated cards or phone reminders will fix it.
Srikanth BH November 28, 2025
Hey, if you’re on warfarin and you’re reading this-first off, you’re already doing better than most. Just by being here, you’re showing up for yourself. That matters. A lot.
I know it feels overwhelming. Like every pill is a landmine. But you’re not alone. I’ve been on warfarin for eight years. I’ve had my INR spike after amoxicillin. I’ve panicked. I’ve cried. I’ve called my clinic at midnight. And guess what? I’m still here. And you will be too.
The key isn’t memorizing every drug. It’s building a team. Your pharmacist? They’re your secret weapon. Tell them you’re on warfarin. They’ll flag everything. Your doctor? They’re not perfect. But they want you safe. Just ask: ‘Is this safe?’ It’s not a dumb question. It’s the smartest one you can ask.
And if you’re scared? That’s okay. But don’t let fear stop you from living. Go to the dentist. Get your antibiotics. Take your warfarin. Just check your INR. That’s it. One test. That’s all it takes to stay safe. You’ve got this.
Jennifer Griffith November 29, 2025
ok so like... bactrim bad? i thought it was just for utis? and why is azithromycin good? isnt that the one that gives you diarrhea? also i took amoxicillin last month and my INR was fine so idk why everyone is freaking out. also can i just take vitamin k pills instead of checking my INR? just asking.
Roscoe Howard November 29, 2025
It’s appalling that this article even exists. In a country where we have the most advanced medical system on Earth, we’re reduced to debating whether a patient should check their INR after taking a simple antibiotic. This is not science. This is bureaucratic chaos. We’ve replaced clinical judgment with algorithmic checklists. We’ve turned physicians into compliance officers. And we’ve made patients into data points. The fact that a 2012 study is still being cited as gospel is a testament to how stagnant our medical guidelines have become. We need innovation-not memorization. We need personalized medicine-not one-size-fits-all warnings. And we need to stop treating patients like children who can’t handle the truth. The truth is: every patient is different. Some can take Bactrim without issue. Others can’t. But we don’t trust them to know. We don’t trust their doctors. We trust a spreadsheet. That’s not healthcare. That’s fearmongering dressed in white coats.
And yet, we still have people like you, reading this, terrified of a pill. That’s not the fault of the medication. It’s the fault of a system that has lost its soul.
Kimberley Chronicle December 1, 2025
From a clinical pharmacology perspective, this is a beautifully nuanced summary. The tripartite mechanism of interaction-CYP2C9 inhibition, gut microbiota disruption, and protein binding displacement-is elegantly articulated. What’s particularly compelling is the differential risk stratification: Bactrim’s triple-hit profile versus clindamycin’s near-zero pharmacokinetic interference. The rifampin paradox is also a masterclass in enzyme induction kinetics-most clinicians overlook the delayed onset and washout period, which can span up to 60 days. I’d only add that vancomycin, while not mentioned, has emerging data suggesting mild INR elevation via gut flora modulation, particularly in prolonged courses. Also, the role of probiotics in mitigating vitamin K depletion is underexplored-some RCTs suggest Lactobacillus strains may help stabilize INR fluctuations during antibiotic exposure. Still, the core message remains unshakable: vigilance, not avoidance. Monitoring is the bridge between safety and autonomy.
Shirou Spade December 1, 2025
Warfarin isn’t a curse. It’s a mirror. It shows you how fragile balance is. How one tiny molecule can change everything. Antibiotics? They’re not enemies. They’re just... strangers walking into your body. They don’t know your story. They don’t know your liver, your gut, your clotting factors. But you do. That’s the power. You’re not passive. You’re the one who holds the map. You’re the one who asks the question. You’re the one who checks the number. And that’s not fear. That’s wisdom.
People say ‘don’t panic.’ But I think panic is okay. Panic means you care. The problem isn’t panic. It’s silence. The silence when you don’t ask. The silence when you don’t check. The silence when you assume. Don’t be silent. Speak. Ask. Check. Even if it’s inconvenient. Even if it’s scary. Even if you feel fine. You’re not just managing a drug. You’re managing your life. And that’s worth every extra blood draw.
Lisa Odence December 2, 2025
Okay, I just want to say-this is THE most helpful article I’ve ever read on warfarin 🥹💖 I’ve been on it since 2020 and I didn’t even know rifampin could make your INR DROP. Like, WHAT?! 😱 I thought all antibiotics made it go up. I’m so glad I read this before my TB exposure screening next week. I’m printing this out and laminating it 📄✨ I’m also downloading the UCSD review and saving it to my phone. I’ve already sent it to my mom (she’s on warfarin too) and my dentist. I even made a note in my Apple Health: ‘NO BACTRIM. YES TO CLINDAMYCIN.’ 💪🩸 I’m not scared anymore-I’m empowered. Thank you for writing this. I’m going to start checking my INR 3 days after every antibiotic now. No more guessing. No more ‘I’m fine.’ I’m done with that. I’m a warfarin warrior now. 🦸♀️💙
Sharley Agarwal December 2, 2025
And yet, people still take Bactrim like it’s a vitamin. Pathetic.