Why accurate cancer staging depends on the right imaging tool
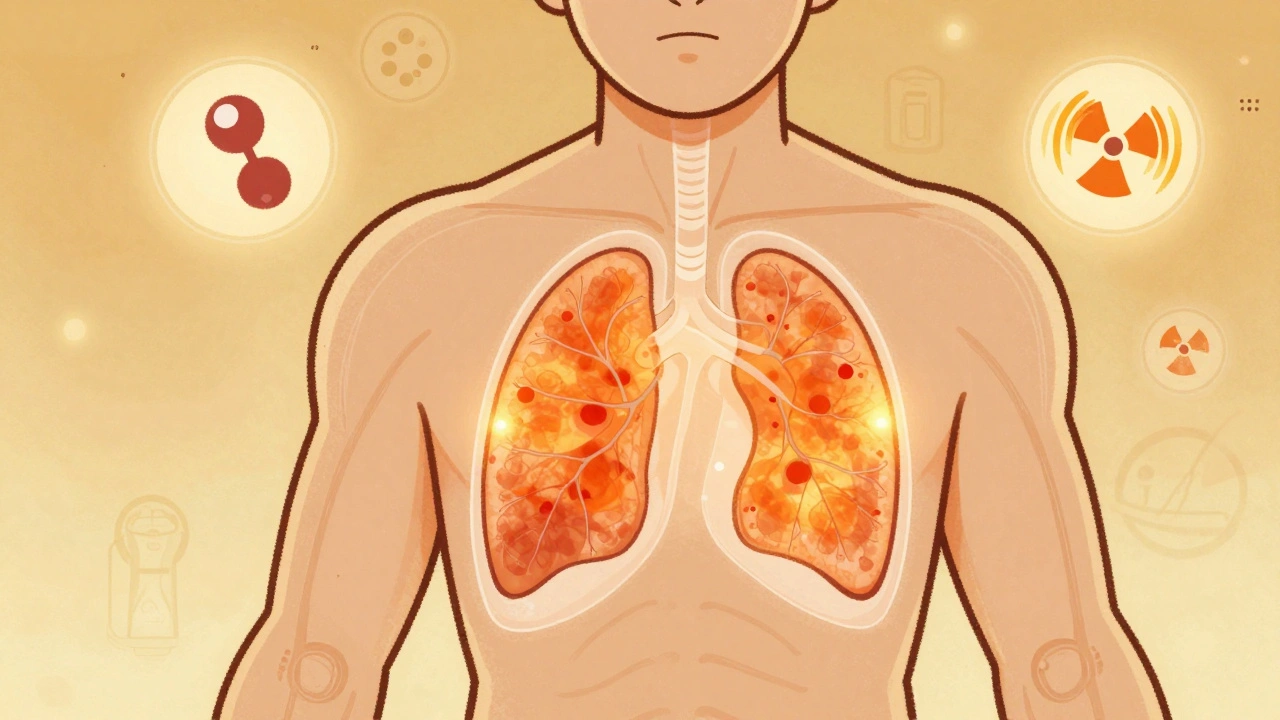
Getting cancer staged right isn’t just important-it can mean the difference between life and death. Staging tells doctors how far the cancer has spread, which directly shapes treatment. Too little staging, and you miss hidden tumors. Too much, and you expose patients to unnecessary radiation or delays. That’s where imaging comes in. Not all scans are created equal. PET-CT, MRI, and PET-MRI each bring something unique to the table. Choosing the right one isn’t about which is "better," but which fits the cancer type, location, and patient needs.
PET-CT: The workhorse of cancer staging
PET-CT has been the go-to for oncology since the early 2000s. It combines two scans: one that shows where cancer cells are metabolically active (PET), and another that gives detailed anatomy (CT). The PET side uses a sugar-based tracer, usually 18F-FDG, that cancer cells gobble up like fuel. This makes tumors light up on the scan, even if they’re too small to see on a regular CT. The CT part pins those glowing spots to exact locations in the body.
It’s fast. A full-body scan takes about 15 to 20 minutes. It’s widely available. Most hospitals have one. And it works well for many cancers-lung, lymphoma, melanoma, and colorectal. In non-small cell lung cancer, PET-CT changes treatment plans in nearly 30% of cases by finding hidden spread that other scans miss.
But it’s not perfect. It struggles with cancers that don’t use much sugar, like some prostate or kidney tumors. It also can’t tell the difference between a tumor and inflammation, which can lead to false positives. And it exposes patients to radiation-around 10 to 25 mSv per scan, similar to several years of natural background radiation.
MRI: The detail master for soft tissue
MRI doesn’t use radiation. Instead, it uses powerful magnets and radio waves to create images based on water content in tissues. This gives it unmatched clarity for soft tissues-brain, spinal cord, liver, prostate, and pelvic organs. That’s why it’s the gold standard for prostate cancer staging. A 2022 study showed MRI detected prostate cancer with 75% accuracy, beating standard PSMA PET-CT at 62%.
MRI also excels at spotting small liver metastases and distinguishing between scar tissue and recurring tumors after radiation. For brain tumors, it’s irreplaceable. It can tell if a dark spot is new cancer or just radiation damage-a critical distinction that affects whether a patient gets more treatment or just monitoring.
The downside? Time. A full MRI can take 30 to 60 minutes. Patients have to lie perfectly still. Motion ruins the images. It’s also not good for people with metal implants-pacemakers, cochlear implants, or certain surgical clips can make MRI unsafe. And while it’s great for anatomy, it doesn’t show metabolic activity. That’s why it’s often paired with PET.

PET-MRI: The hybrid future, but not for everyone
PET-MRI came onto the scene around 2011. It’s a single machine that does both PET and MRI at the same time. That means one appointment, one set of images fused perfectly together. No moving the patient between machines. No misalignment. For complex cases, this is powerful.
It’s especially useful in three areas: brain tumors, pelvic cancers (like cervical or rectal), and pediatric cases. For brain tumors, PET-MRI correctly identifies recurrence versus radiation necrosis 85-90% of the time, compared to 70-80% for MRI alone. In children, it cuts radiation exposure by about half compared to PET-CT, which matters when they’ll need scans over many years.
But it’s not a magic bullet. It’s expensive-up to 50% more than PET-CT. A single scan can cost $2,500 to $3,500. The machine itself costs over $4 million. Fewer than 1 in 5 cancer centers in the U.S. have one. And it’s slower. Scans take 45 to 60 minutes. That’s tough for frail patients or those in pain.
Technologists need extra training. Radiologists need to learn how to interpret both metabolic and soft-tissue data together. And there’s a technical headache: getting the PET signal accurate inside the MRI’s magnetic field requires advanced software. Many centers still struggle with artifacts that can blur results.
How experts choose between them
There’s no one-size-fits-all rule. Experts follow a simple principle: match the tool to the cancer and the question.
For lung cancer staging? PET-CT is still first-line. It’s fast, proven, and finds distant spread well.
For prostate cancer? Multiparametric MRI is now standard for initial diagnosis. PSMA PET-CT is added if the cancer is aggressive or if PSA rises after treatment.
For breast cancer after chemo? PET-CT gives better specificity early in treatment-meaning fewer false alarms. But MRI is better at measuring tumor shrinkage over time.
For liver or pancreatic cancer? PET-MRI is becoming the preferred option. It spots small lesions better than either scan alone. One 2023 study found PET-MRI changed treatment plans for nearly half of pancreatic cancer patients.
For kids or young adults needing long-term follow-up? PET-MRI’s lower radiation makes it the smarter long-term choice-even if it’s harder to schedule.

What’s changing in 2025
Technology is moving fast. In January 2024, Siemens got FDA clearance for a new PET-MRI system that cuts scan time to just 6 minutes for a full-body scan. That’s a game-changer. It could make PET-MRI more practical for busy clinics.
Artificial intelligence is also stepping in. New algorithms can analyze PET and MRI data to predict how a tumor will respond to treatment before the patient even gets their next scan. The NCI’s PREDICT trial is testing whether AI can pick the best therapy based on imaging patterns alone.
And new tracers are coming. While 18F-FDG is still the standard, tracers like 68Ga-PSMA-11 (for prostate cancer) and 68Ga-DOTATATE (for neuroendocrine tumors) are becoming more common. These bind to specific cancer markers, making tumors glow brighter and more accurately.
Practical realities for patients and providers
For patients: Ask your doctor why they’re recommending a specific scan. Don’t assume more expensive means better. If you’re young, or need repeated scans, ask about radiation exposure. If you have metal implants, confirm MRI is safe.
For providers: Don’t force a PET-MRI just because you have one. Use it where it adds real value. For routine lung cancer staging, PET-CT is still faster, cheaper, and just as accurate. Save PET-MRI for the cases where soft tissue detail or lower radiation makes a clinical difference.
Cost and access still limit use. In the U.S., only academic centers and large hospitals have PET-MRI. In the UK and Europe, adoption is slower due to funding constraints. Even where available, insurance often requires pre-authorization. The key is knowing when to use it-and when not to.
Bottom line: Right tool, right time
PET-CT, MRI, and PET-MRI aren’t rivals-they’re teammates. Each has strengths and limits. The goal isn’t to pick the "best" scan. It’s to pick the right one for the patient in front of you.
For most cancers, PET-CT remains the backbone. For soft tissue detail, MRI is unmatched. For complex cases where precision matters most, PET-MRI offers a clear edge. And as technology improves, the lines will blur even further. But for now, the most accurate staging comes not from the machine, but from the clinical judgment behind it.




12 Comments
Arun kumar December 2, 2025
i love how this breaks it down without jargon overload. pet-ct is like the trusty old truck that gets you there, but sometimes you need a luxury suv with leather seats (pet-mri) for the rough terrain. also, who knew cancer cells are basically sugar addicts? 🤯
Zed theMartian December 4, 2025
Let me guess-this was written by someone who thinks 'radiation exposure' is a buzzword invented by Big Pharma to sell MRIs. The truth? PET-CT saves lives. MRI is just a fancy camera that takes 45 minutes to tell you what a $500 CT already showed. If you're not using PET-CT as your baseline, you're not practicing medicine-you're performing art.
Ella van Rij December 5, 2025
Ohhh so PET-MRI is 'the future'... but only if you're rich, have a 3-hour window, and don't mind your insurance denying it because 'it's not medically necessary'... again. I swear, if one more person tells me 'it's about clinical judgment' I'm going to scream into a PET scanner. 😌
ATUL BHARDWAJ December 6, 2025
In India we wait 6 months for a CT. PET is a dream. MRI? Only in Mumbai. But still, the point stands. Tool fits the need. Not the other way around.
Steve World Shopping December 6, 2025
The fundamental flaw in this narrative is the conflation of modality specificity with clinical utility. PET-CT provides metabolic-topological corroboration, whereas MRI delivers high-resolution soft-tissue contrast with superior spatial fidelity. PET-MRI, as a multimodal fusion platform, enables simultaneous spatiometabolic phenotyping-critical for precision oncology. Failure to adopt this paradigm constitutes diagnostic negligence.
Rebecca M. December 7, 2025
I just had my third PET-CT this year and my insurance company sent me a letter that said 'We noticed you're alive. Please stop.' I'm 29. I have cancer. And I'm being punished for surviving. So yeah, let's talk about radiation. Let's talk about it ALL THE TIME.
Lynn Steiner December 9, 2025
I just got my PET-MRI results and I'm crying. Not because of the cancer-because the machine was so loud I thought I was in a metal drum. And then the tech said 'you're doing great!' like I'm a puppy. I just want to know if it's spread or not. Not a spa day. 😭
Alicia Marks December 10, 2025
This is such a helpful breakdown. You're right-it's not about the machine, it's about the person. If you're a kid or someone who needs scans every year, lowering radiation matters. And if you're in pain, 60 minutes on a hard table? That’s a whole other battle. Thank you for seeing the human behind the scan.
Paul Keller December 11, 2025
While I appreciate the general overview, I must emphasize that the current clinical guidelines from NCCN and ESMO continue to endorse PET-CT as the standard of care for initial staging in non-small cell lung cancer, with MRI reserved for specific scenarios such as suspected brain or adrenal metastases. The notion that PET-MRI is 'preferred' for pancreatic cancer remains controversial and is not yet reflected in major consensus guidelines. The cited 2023 study, while intriguing, is single-center and retrospective-its generalizability is limited without prospective validation.
Shannara Jenkins December 13, 2025
I'm a radiology tech and I see this every day. The hardest part isn't the tech-it's the patients who think 'more expensive = better'. I had one guy refuse PET-CT because he thought MRI was 'purer'. We ended up doing both. He cried when he found out the PET-CT found the tumor the MRI missed. Sometimes the simple tool saves the day.
Laura Baur December 13, 2025
I find it deeply concerning that this article casually dismisses the ethical implications of routine PET-CT use in young patients. The linear no-threshold model of radiation carcinogenesis suggests that even low-dose exposures carry cumulative stochastic risk. By normalizing 10-25 mSv scans in patients who may require multiple studies over decades, we are essentially trading a known, quantifiable risk of secondary malignancy for the illusion of diagnostic certainty. This is not medicine-it is institutionalized risk normalization disguised as pragmatism. The medical community must confront its complicity in this slow-burn public health crisis.
Jack Dao December 13, 2025
You people act like PET-MRI is some kind of miracle. I work at a rural hospital. We don’t have one. We don’t even have a working MRI half the time. Meanwhile, you’re all up in arms about radiation when the real issue is that 80% of the world doesn’t even have access to a basic CT. So stop pretending this is about 'precision'. It’s about privilege.